
Table of Contents
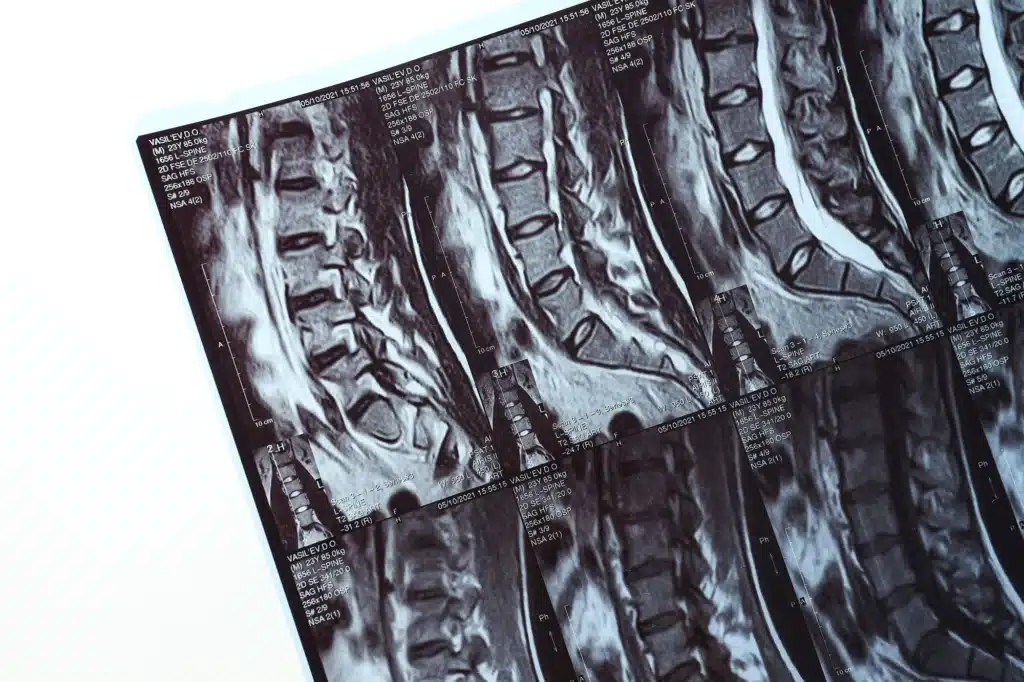
ToggleSpinal stenosis is a condition where the spaces within your spine narrow, putting pressure on the nerves that travel through the spine. This condition can occur anywhere along the spine but is most common in the lower back and neck.
Causes of spinal stenosis include age-related changes, arthritis, herniated disks, thickened ligaments, and spinal injuries. Patients with spinal stenosis often experience symptoms like back pain, numbness, tingling, muscle weakness, and impaired mobility.
These symptoms can significantly impact daily activities and quality of life, making effective treatment essential.

Traditional spine surgery, also known as open surgery, involves making a long incision down the back, through which the surgeon can access the spine. This approach often requires moving and sometimes cutting muscles and soft tissues to reach the problem area.
In contrast, minimally invasive spine surgery (MISS) uses smaller incisions and specialized instruments to minimize muscle and tissue damage. During MISS, a tubular retractor is used to create a tunnel to the spine, allowing the surgeon to work through a smaller operative field.
This results in less pain, a shorter hospital stay, and a quicker recovery compared to traditional surgery.
Minimally invasive spine surgery offers several benefits over traditional surgery, especially for treating spinal stenosis. Firstly, there is reduced muscle and tissue damage, leading to less postoperative pain and a quicker recovery.
Patients typically experience a shorter hospital stay, often going home the same day or within a couple of days. There is also a lower risk of infection due to smaller incisions and reduced blood loss during surgery.
Additionally, the cosmetic results are better, with smaller scars compared to the large scar from traditional surgery. Overall, these benefits contribute to a faster return to daily activities and an improved quality of life.
Not everyone with spinal stenosis is a candidate for minimally invasive spine surgery. Ideal candidates are those with specific conditions that have not responded to non-surgical treatments such as medication, physical therapy, or chiropractic care.
Conditions suitable for MISS include herniated disks, spinal tumors, vertebral fractures, and certain spinal deformities. Patients should be in good overall health and not have any medical conditions that would complicate surgery.
A thorough evaluation by a spine specialist is necessary to determine if MISS is the right option. This evaluation includes imaging tests like X-rays or MRIs and a review of the patient’s medical history and current symptoms.
There are several minimally invasive techniques used to treat spinal stenosis. One common method is the use of tubular retractor systems, which involve dilating the soft tissues to create a small tunnel to the spine.
This technique minimizes muscle damage and allows the surgeon to perform the procedure through a small incision. Another technique is the percutaneous placement of screws and rods, used to stabilize the spine without the need for large incisions.
Endoscopic procedures use a camera and small instruments inserted through tiny incisions to treat the spine. Lateral access routes involve approaching the spine from the side of the body, which is beneficial for lumbar spine surgeries. Thoracoscopic approaches allow access to the thoracic spine through small incisions in the chest.
What Can Patients Expect During the Recovery Process After Minimally Invasive Spine Surgery?
The recovery process after minimally invasive spine surgery is typically quicker and less painful compared to traditional open surgery. Patients can usually expect a shorter hospital stay, often going home the same day or within a couple of days.
Pain management is crucial during the initial recovery period and can be effectively handled with prescribed pain medications, cold packs, and regular, gentle walking to promote healing.
Physical therapy plays a significant role in the recovery process. It helps patients regain strength, improve mobility, and return to their daily activities more quickly.
Most patients can resume light activities within a few weeks, but complete recovery might take several months depending on the specific procedure and the patient’s overall health. It is important to follow all postoperative instructions provided by your healthcare provider to ensure a smooth recovery and minimize the risk of complications.
For more detailed information on the importance of physical therapy after spine surgery, you can read this article.

Like any surgical procedure, minimally invasive spine surgery carries certain risks and complications. Common risks include infection, blood clots, and adverse reactions to anesthesia.
Specific risks of MISS include nerve damage, spinal fluid leaks, and insufficient pain relief. While these complications are rare, it is important for patients to be aware of them and discuss them with their surgeon before the procedure.
Choosing an experienced surgeon and a well-equipped surgical facility can help minimize these risks. Patients should also follow all preoperative and postoperative instructions to reduce the likelihood of complications.
Minimally invasive spine surgery has been shown to be highly effective in treating spinal stenosis. Studies have demonstrated that patients who undergo MISS experience significant pain relief, improved mobility, and a better quality of life compared to those who do not have surgery.
The success rates of MISS are comparable to those of traditional surgery, with the added benefits of quicker recovery and less postoperative pain. Long-term outcomes are also favorable, with many patients experiencing sustained improvement in their symptoms.
However, the effectiveness of the surgery depends on the individual patient and the severity of their condition.
Preparing for minimally invasive spine surgery involves several important steps. Patients should stop smoking and engage in regular exercise to improve their overall health and shorten recovery time.
It is essential to review all medications and supplements with the surgical team, as some may need to be discontinued before the surgery. Preoperative imaging tests such as X-rays or MRIs will be ordered to guide the surgery.
Patients should follow instructions regarding fasting before surgery and inform their healthcare provider of any changes in their health, such as a fever. Proper preparation helps ensure a smooth surgery and recovery.

Choosing the right surgeon for minimally invasive spine surgery is crucial for a successful outcome. Patients should look for a surgeon with extensive experience and specialized training in MISS techniques.
Board certification and credentials in spine surgery are important indicators of a surgeon’s qualifications. It is also beneficial to choose a surgeon who is affiliated with a reputable hospital or surgical center equipped with advanced technology.
Patients should ask about the surgeon’s success rates and patient outcomes, as well as the number of MISS procedures they have performed. Personal recommendations and patient reviews can also provide valuable insights.
For more information about our team of experienced spine surgeons, please visit the Long Island Neuroscience Specialists website. Our team has over 30 years of experience in brain and spine surgery, ensuring the highest quality of care for our patients.
In conclusion, minimally invasive spine surgery for spinal stenosis offers numerous benefits, including reduced muscle and tissue damage, less postoperative pain, shorter hospital stays, and quicker recovery times. This advanced surgical technique has proven to be highly effective in treating spinal stenosis, providing patients with significant pain relief and improved quality of life.
If you are considering spine surgery for spinal stenosis, it is important to consult with a qualified spine specialist to determine if you are a good candidate for minimally invasive spine surgery. Proper preparation and choosing an experienced surgeon are crucial for a successful outcome.
At Long Island Neuroscience Specialists, our team of experienced spine surgeons is dedicated to providing the highest quality of care to our patients. With over 30 years of experience in brain and spine surgery, we are committed to helping you achieve the best possible results.
For more information or to schedule a consultation, please visit our doctors or contact us today.
GET IN TOUCH +
285 Sills Road
Building 5-6, Suite E
East Patchogue, NY 11772
(631) 475-5511
184 N. Belle Mead Road
East Setauket, NY 11733
(631) 675-6226
GET IN TOUCH +
285 Sills Road
Building 5-6, Suite E
East Patchogue, NY 11772
(631) 475-5511
184 N. Belle Mead Road
East Setauket, NY 11733
(631) 675-6226
SUBSCRIBE TO OUR NEWSLETTER +
Send us a Google review. Click this link and let us know how we did!
Review us on Yelp too.