
Table of Contents
ToggleAs a spine surgeon with over 25 years of experience, I have seen countless patients struggle with pain that affects their quality of life. For many, the right solution involves opioids.
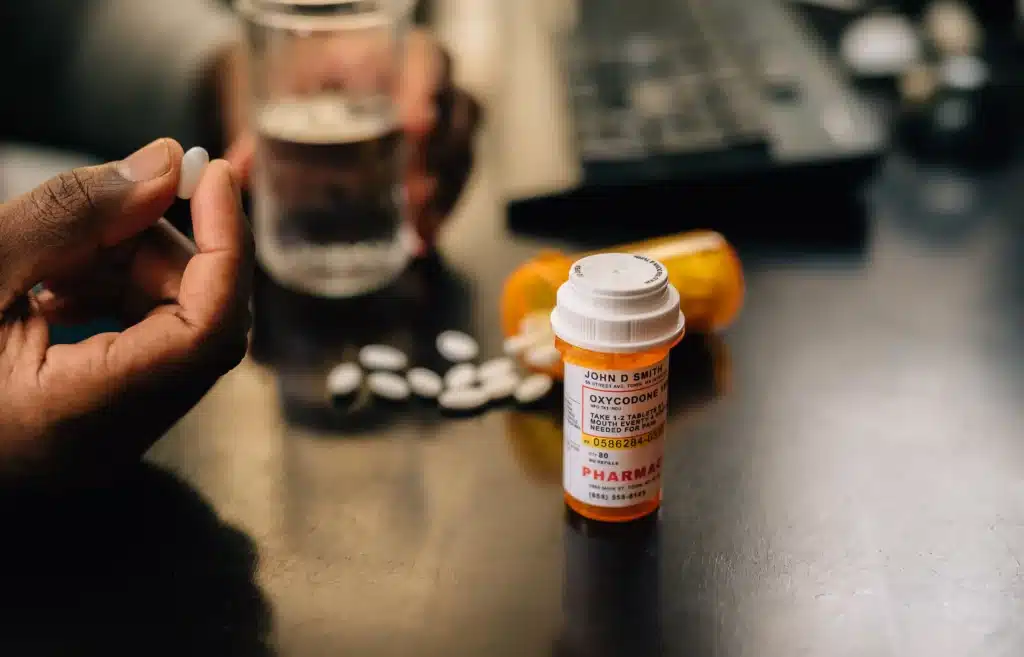
Opioid benefits for pain are undeniable when they’re used correctly. These medications work by binding to receptors in the brain, blocking pain signals, and even creating feelings of relief and comfort.
Unlike other pain relievers, opioids target severe pain at its source, making them invaluable in specific medical contexts. When we talk about opioids, we’re referring to a class of drugs that includes medications like morphine, oxycodone, and fentanyl.
They can be natural (derived from the poppy plant) or synthetic (produced in labs). Their primary purpose is to alleviate intense pain, often in scenarios where other treatments fall short.
However, understanding how to use them safely and effectively is key to harnessing their full potential
One of the most frequent questions I hear is, “When should opioids be used for pain management?” Over the years, I’ve learned that opioids shine in very specific circumstances. Post-surgical recovery is one of the most common scenarios.
After spinal surgeries, where the body undergoes significant trauma, opioids can provide the relief necessary to jumpstart recovery. They allow patients to rest, regain mobility, and avoid complications associated with unmanaged pain.
For chronic conditions like cancer-related pain or severe arthritis, opioids can be life-changing. In these cases, pain isn’t just a momentary discomfort—it’s a constant presence that can wear down a person’s physical and emotional resilience.
I’ve seen opioids give these patients the freedom to move, work, and enjoy life again. In palliative care, they’re a cornerstone for ensuring dignity and comfort in the final stages of life.
Acute injuries, such as fractures or burns, are another area where opioids are invaluable. They’re often prescribed as a short-term solution to manage severe pain while the body heals. The goal is to use the lowest effective dose for the shortest duration, ensuring relief without unnecessary risk.
The science behind opioid benefits for pain is fascinating. Opioids interact with the body’s central nervous system by binding to specific receptors in the brain and spinal cord.
These receptors, called mu, kappa, and delta receptors, are part of a natural system designed to control pain. When opioids activate these receptors, they block pain signals, providing significant relief.
Additionally, opioids can reduce the emotional response to pain. This dual effect makes them particularly effective for conditions that involve both physical discomfort and emotional distress, such as chronic back pain or post-operative recovery.
Some opioids, like methadone, also have unique mechanisms, such as NMDA receptor antagonism, which make them especially useful for neuropathic pain. This targeted action explains why opioids are often the go-to choice for severe pain.
However, it also underscores the importance of careful management. Misuse can disrupt this delicate balance, leading to side effects or addiction.
That’s why healthcare providers play such a vital role in overseeing opioid therapy.
When it comes to severe pain, opioids often outperform alternatives. First, their rapid onset of action provides near-immediate relief, which is critical in acute scenarios like surgery or trauma.
Second, they’re versatile, available in various forms such as pills, patches, or injections, to suit different medical needs. Another significant advantage is their effectiveness in treating pain that’s resistant to other medications.
For example, NSAIDs like ibuprofen may help with mild inflammation but often fall short in addressing the deep, persistent pain of conditions like herniated discs or cancer. Opioids bridge this gap, offering a level of relief that other drugs can’t match.
In addition, opioids can be combined with non-opioid therapies for a synergistic effect. For instance, pairing them with physical therapy or regional anesthetics often yields better outcomes than using opioids alone.
This integrative approach helps patients regain function more quickly and with fewer complications.

One of the most critical aspects of opioid therapy is responsible use. As a physician, I’ve seen how education can make all the difference.
Patients who understand their treatment plan—including dosage, duration, and potential risks—are far less likely to encounter problems. The key is to start with the lowest effective dose and to use opioids only as long as necessary.
For example, after spinal surgery, I might prescribe a short course of opioids to manage immediate post-operative pain, supplemented by non-opioid medications and physical therapy. Regular follow-ups ensure that we adjust the treatment as needed, reducing reliance on opioids over time.
Patients should also be aware of the early signs of misuse or dependence. Symptoms like needing higher doses to achieve the same relief or using opioids for non-medical reasons are red flags that require immediate attention.
Open communication with healthcare providers is essential for addressing these issues promptly.
Like any powerful medication, opioids come with risks. Common side effects include nausea, constipation, and drowsiness, which are often manageable with proper care.
However, higher doses can lead to more severe complications like respiratory depression, which is why dosing must be carefully monitored. Long-term use increases the risk of tolerance, where the body becomes less responsive to the medication, and dependence, where withdrawal symptoms occur if the drug is stopped suddenly.
In rare cases, opioids can even heighten pain sensitivity, a condition known as opioid-induced hyperalgesia. These risks highlight the importance of using opioids under strict medical supervision.
With the right precautions, such as regular check-ups and a clear plan for tapering off the medication, most patients can avoid these complications.
While opioid benefits for pain are significant, they’re not the only option. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or acetaminophen are effective for mild to moderate pain.
For localized pain, regional anesthetics can provide relief without systemic effects. Nonpharmacological approaches also play a vital role.
Physical therapy, acupuncture, and even mindfulness techniques can complement opioid therapy, reducing the need for higher doses. In my practice, I’ve seen how these methods can accelerate recovery, particularly when integrated into a broader treatment plan.
Cognitive-behavioral therapy (CBT) is another valuable tool, especially for chronic pain. By addressing the psychological aspects of pain, CBT can improve patients’ overall well-being and make them less reliant on medication. Read more here.

As healthcare providers, we are the gatekeepers of safe opioid use. Our role begins with assessing whether opioids are the right choice for a patient’s pain.
This involves weighing the benefits against the risks, considering factors like medical history, current medications, and potential for misuse. Monitoring is an ongoing responsibility.
Regular follow-ups allow us to adjust treatment as needed, ensuring that opioids remain effective without becoming problematic. Tools like prescription drug monitoring programs (PDMPs) help track usage and identify any red flags.
Education is equally crucial. By informing patients about proper use, potential risks, and alternatives, we empower them to make informed decisions about their care.
Despite our best efforts, some patients may struggle with opioid misuse. Recognizing the signs early can make all the difference.
These include taking higher doses than prescribed, showing withdrawal symptoms, or using opioids for emotional relief rather than physical pain. Resources like the MAT Act have made it easier for patients to access treatment for opioid use disorder.
Medications like buprenorphine, combined with counseling and support, offer a path to recovery. The key is to address the issue without stigma, fostering a supportive environment for healing.
Opioid therapy is governed by stringent guidelines to ensure safety and effectiveness. The CDC recommends using the lowest effective dose for the shortest possible duration, particularly for acute pain.
These guidelines are designed to minimize risks while ensuring that patients receive adequate relief. State-level prescription drug monitoring programs are another critical tool.
They help track opioid prescriptions and identify patterns that may indicate misuse or diversion. In my practice, I’ve found these programs invaluable for ensuring that opioids are used responsibly.
Collaborative care models also play a role. By involving pharmacists, physical therapists, and other healthcare professionals, we create a comprehensive plan that addresses all aspects of pain management.
This team-based approach not only improves outcomes but also reduces the likelihood of complications. Read more here.

The most effective use of opioids occurs within a broader pain management strategy. This means combining medications with nonpharmacological therapies, lifestyle changes, and ongoing support from healthcare providers.
For example, a patient recovering from spinal surgery might use opioids initially but transition to physical therapy and NSAIDs as their condition improves. Regular reassessment is key.
Pain levels, functional goals, and overall health should guide treatment adjustments. By staying flexible and patient-focused, we can ensure that opioids remain a valuable tool without becoming a burden.
Opioids offer significant benefits for pain management when used responsibly. By understanding their mechanisms, risks, and alternatives, patients and healthcare providers can work together to achieve effective relief.
With over 25 years of experience, I’ve seen firsthand how these medications can transform lives—but only when they’re part of a thoughtful, comprehensive approach to care. For those seeking expert guidance on opioid benefits for pain and other advanced pain management options, our team at Long Island Neuroscience Specialists is here to help.
Together, we can find the solution that works best for you.
GET IN TOUCH +
285 Sills Road
Building 5-6, Suite E
East Patchogue, NY 11772
(631) 475-5511
184 N. Belle Mead Road
East Setauket, NY 11733
(631) 675-6226
GET IN TOUCH +
285 Sills Road
Building 5-6, Suite E
East Patchogue, NY 11772
(631) 475-5511
184 N. Belle Mead Road
East Setauket, NY 11733
(631) 675-6226
SUBSCRIBE TO OUR NEWSLETTER +
Send us a Google review. Click this link and let us know how we did!
Review us on Yelp too.